Referral
Each MMC has their own process for referral and details of who to refer and how can be found by clicking on each centre below. It is recommended that you refer to the centre that is closest to the woman, but if you need any guidance please see table below for hospitals and which locality they sit in. For advice about the most appropriate centre for a specific condition, please contact the team to discuss.

St Mary's Hospital - Manchester

Liverpool Women's Hospital

Lancashire Teaching Hospital - Preston
Providers falling within each locality and their MMC are listed below:
| LMNS | Cheshire & Merseyside | Greater Manchester & Eastern Cheshire | Lancashire & South Cumbria |
| MMC | Liverpool Women’s Hospital NHS FT | Manchester University NHS FT St Mary’s Hospital Oxford Road Campus |
Lancashire Teaching Hospital (Preston) |
| Provider Trust’s | Countess of Chester Hospital NHS FT
Mid-Cheshire Hospitals NHS FT (Leighton) Mersey and West Lancashire Teaching Hospitals NHS Trust (St Helens & Knowsley) Mersey and West Lancashire Teaching Hospitals NHS Trust (Southport & Ormskirk) Warrington & Halton Teaching Hospitals NHS FT Wirral University Teaching Hospital NHS FT |
Bolton FT
East Cheshire NHS Trust (Macclesfield) MFT North Manchester General Hospital MFT Wythenshawe Northern Care Alliance NHS FT Stockport NHS FT Tameside & Glossop NHS FT Wrightington, Wigan and Leigh NHS FT |
East Lancashire Hospital NHS Trust
University Hospital Morecambe Bay NHS FT (Furness) University Hospital Morecambe Bay NHS FT (Lancaster) Blackpool Teaching Hospitals NHS FT |
Each MMC provides a regional service including pre-pregnancy, antenatal and postnatal care for women who have either pre-existing significant medical problems or medical problems arising in or shortly after pregnancy. The MMCs also provide advice and care for the most complex and highest risk women.
Medical conditions are classified as category A, B or C depending on complexity and thus provide a guide as to a woman’s care pathway.
These categories are a guide only. They can be modified according to local expertise and experience. Where local expertise is sufficient, a condition may move from category C to B, or B to A. An example would be epilepsy, where there may be a local joint obstetric epilepsy clinic including a neurologist with expertise in epilepsy in pregnancy, in which case care could remain local. Where local expertise is insufficient, when a condition progresses or increases in severity during pregnancy, or when there is clinical concern, a condition should move from category A to B, or B to C:
We strive to ensure that most women with medical complications during pregnancy will continue to be managed by their local maternity hospital within the NW MMN through the provision of outreach clinics. Only a small number of women with complex medical needs will need to receive all their care and give birth at an MMC.
The criteria for referral has been developed using the NHSE Maternal Medicine Service Specification (2021) in consultation with Lead Obstetricians and Physicians from across the network. There have been some amendments to reflect local expertise and services across North West. For details of individual conditions and who to refer please click here.
Referrals and MDT
All providers within the networks footprint will be responsible for agreeing and upholding shared protocols on the management and referral of women with medical conditions, including reviewing guidelines and referral pathways. This model of care will ensure that – where agreed appropriate – investigation and management is carried out by an experienced Multidisciplinary Team (MDT).
Each MMC hosts a specialist MDT comprising of obstetric physicians, specialist physicians, obstetricians, anaesthetists and midwives who have expertise in a range of medical conditions.
The criteria for referral has been developed using the NHSE Maternal Medicine Service Specification (2021) in consultation with Lead Obstetricians and Physicians from across the network. Each MMC has their own process for referral. Details of who to refer and how can be found by clicking on each centre above. It is recommended that you refer to the centre that is closest to the woman, but if you need any advice about the most appropriate centre for a specific condition, please contact the team to discuss.
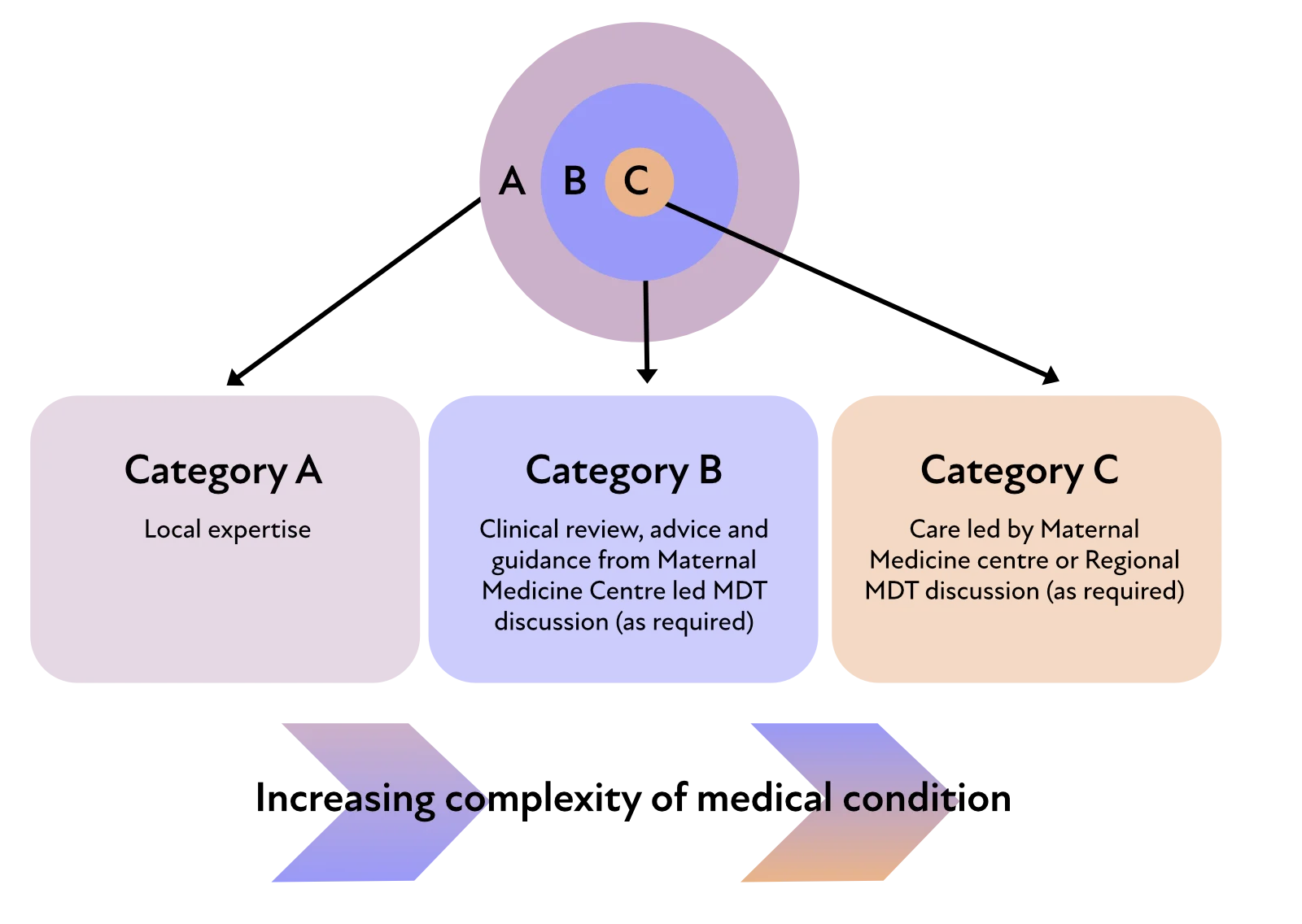
These categories are a guide only. They can be modified according to local expertise and experience. Where local expertise is sufficient, a condition may move from category C to B, or B to A. An example would be epilepsy, where there may be a local joint obstetric epilepsy clinic including a neurologist with expertise in epilepsy in pregnancy, in which case care could remain local. Where local expertise is insufficient, when a condition progresses or increases in severity during pregnancy, or when there is clinical concern, a condition should move from category A to B, or B to C:
When referring women/birthing people, be respectful and aware of all religions, languages, cultures and diversities to ensure best care for all.
Please take into consideration the additional challenges faced by those who are from an ethnic minority, have a severe mental illness or are socially deprived as they are at a higher risk of poor physical health and poor outcomes, compared with the general population.
The perinatal period adds further complexity, therefore please ensure you consider mental health needs and refer to your local perinatal mental health service appropriately.
Each MMC is equipped to facilitate and organise telemedicine across the MMN if it is safe for the woman/birthing person. The option to facilitate consultations via telemedicine is available for pregnancies where it is difficult for the woman/birthing person to attend an appointment in person.
Telemedicine will also be used where expertise is required for specific cases and clinicians from several providers need to work together as a MDT to implement joint care plans.
This mitigates the geographical challenges that occur when experts are not based at the same Trust.
Women of extremely advanced maternal age (>45) or with a raised BMI (>50) in isolation do not meet the requirements for referral to the MMC. However, these women often have co-morbidities.
We recommend an individualised risk assessment and referral to the MMC if there are additional medical conditions or concern.
The majority of women with complications during pregnancy will continue to be managed by local maternity services. The proportion of care delivered by a MMC will vary according to individual need. For some, a single visit to the MMC or communication with the MMC by the local unit will suffice. For the highest risk and most complex cases, it may be that all care will be recommended to be delivered within the MMC.
Referral outcomes
The MDTs are collaborative: the MDT recommendations are based on a discussion with the referrer, taking into account local expertise and concerns, the woman’s preferences and the specialist advice. The aim is to offer comprehensive advice for antenatal, intra-partum and post-partum care.
Practically this means that the recommendation may be for women to continue with their care locally with ongoing MDT input if desired or required, or to transfer their care for investigation, management and / or delivery to a tertiary centre. Our overarching aim is to provide the safest care closest to home.