Services and Referrals
Maternal Medicine Referrals
Maternal Medicine Specialties
Preconceptual Care
Acute medical problems in pregnancy
Post partum care
Medications
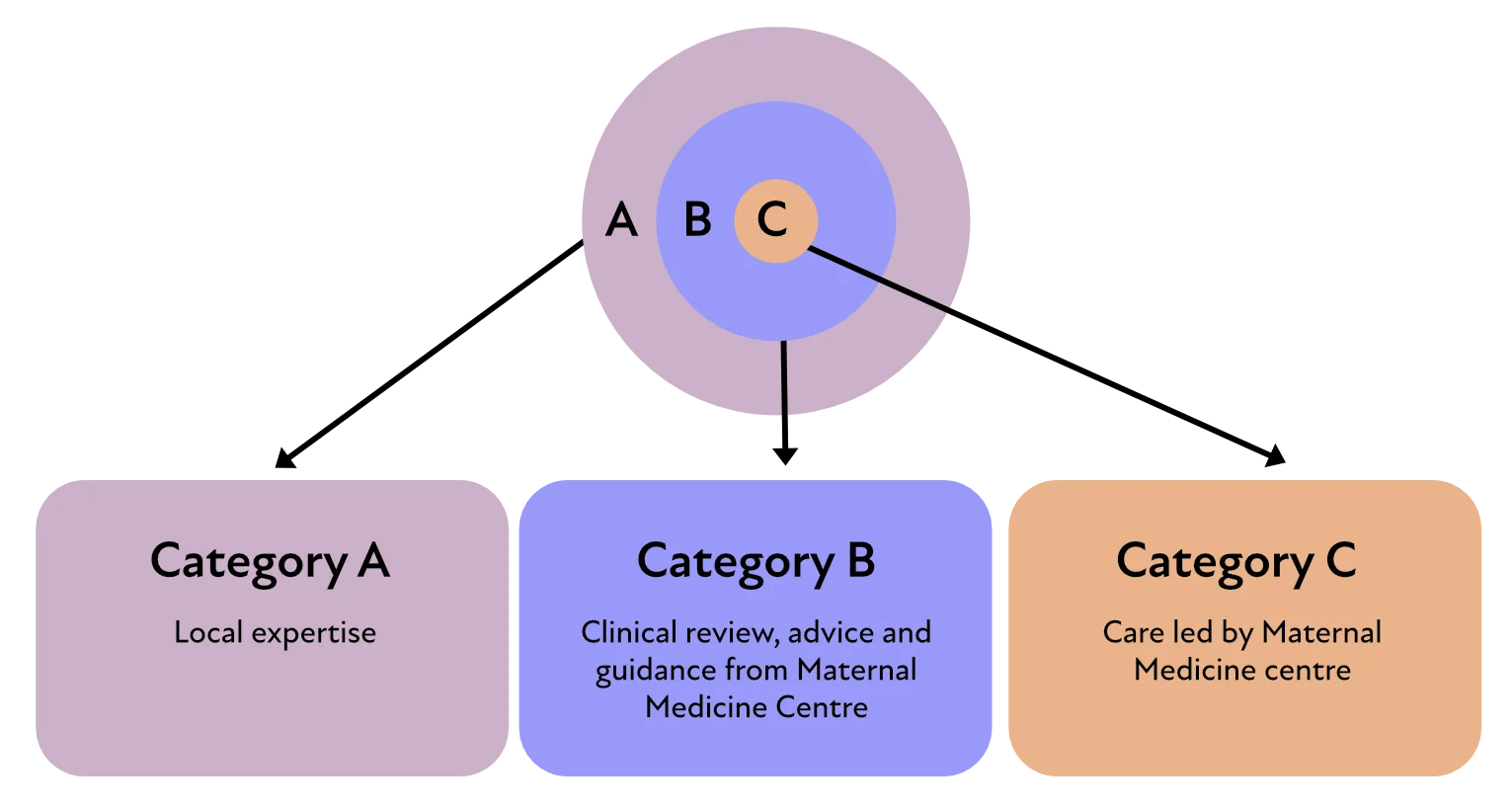
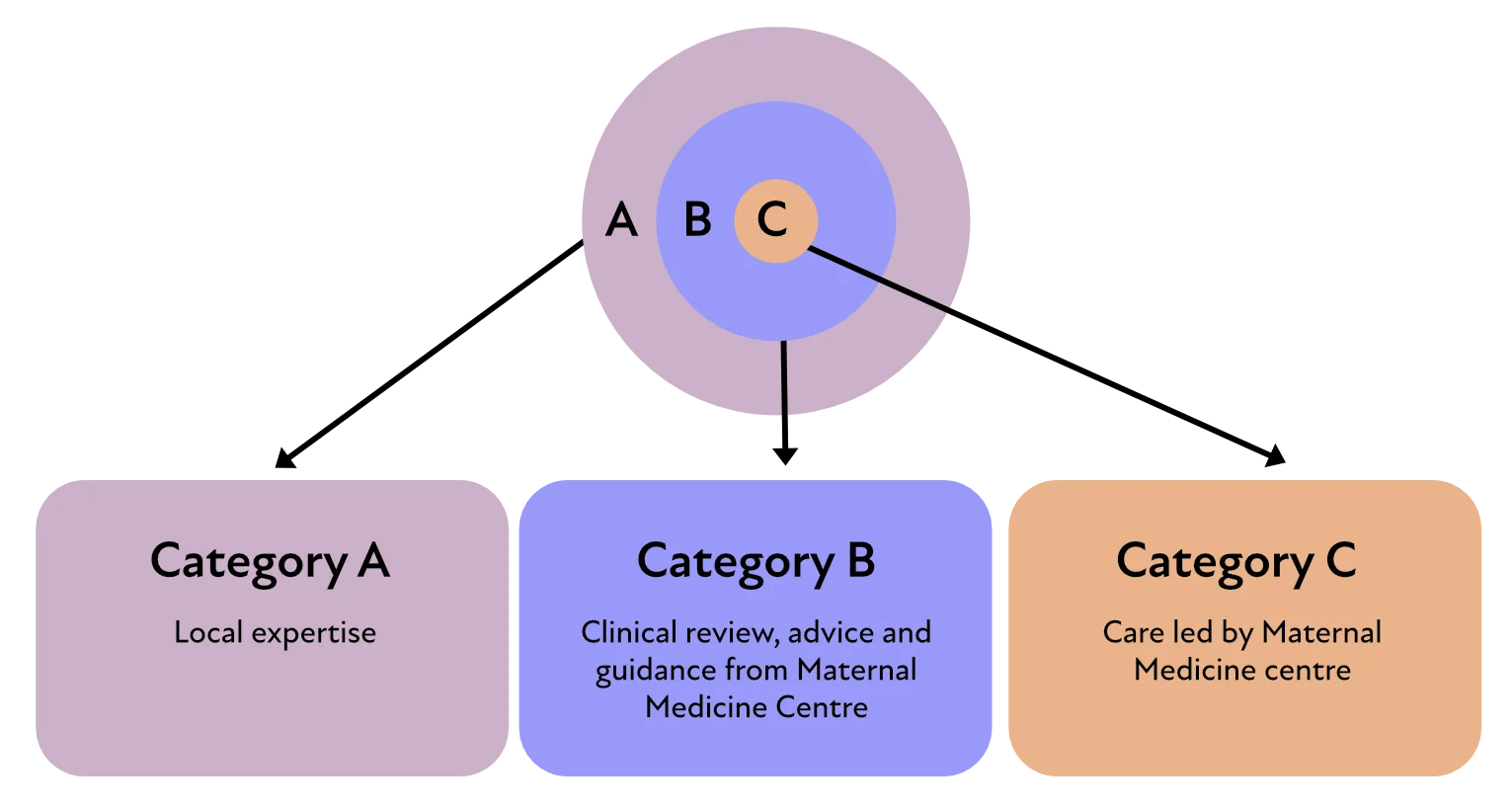
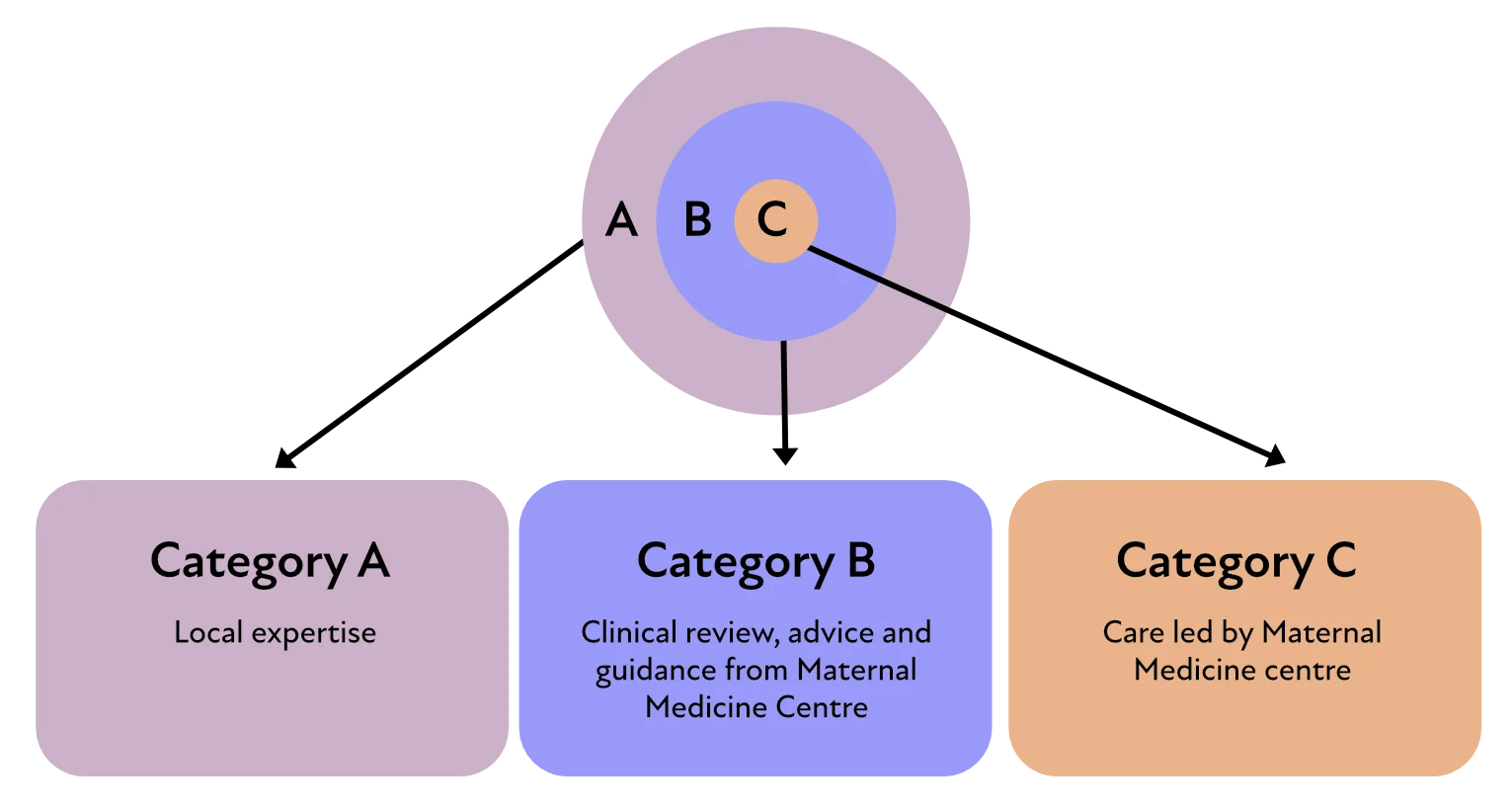
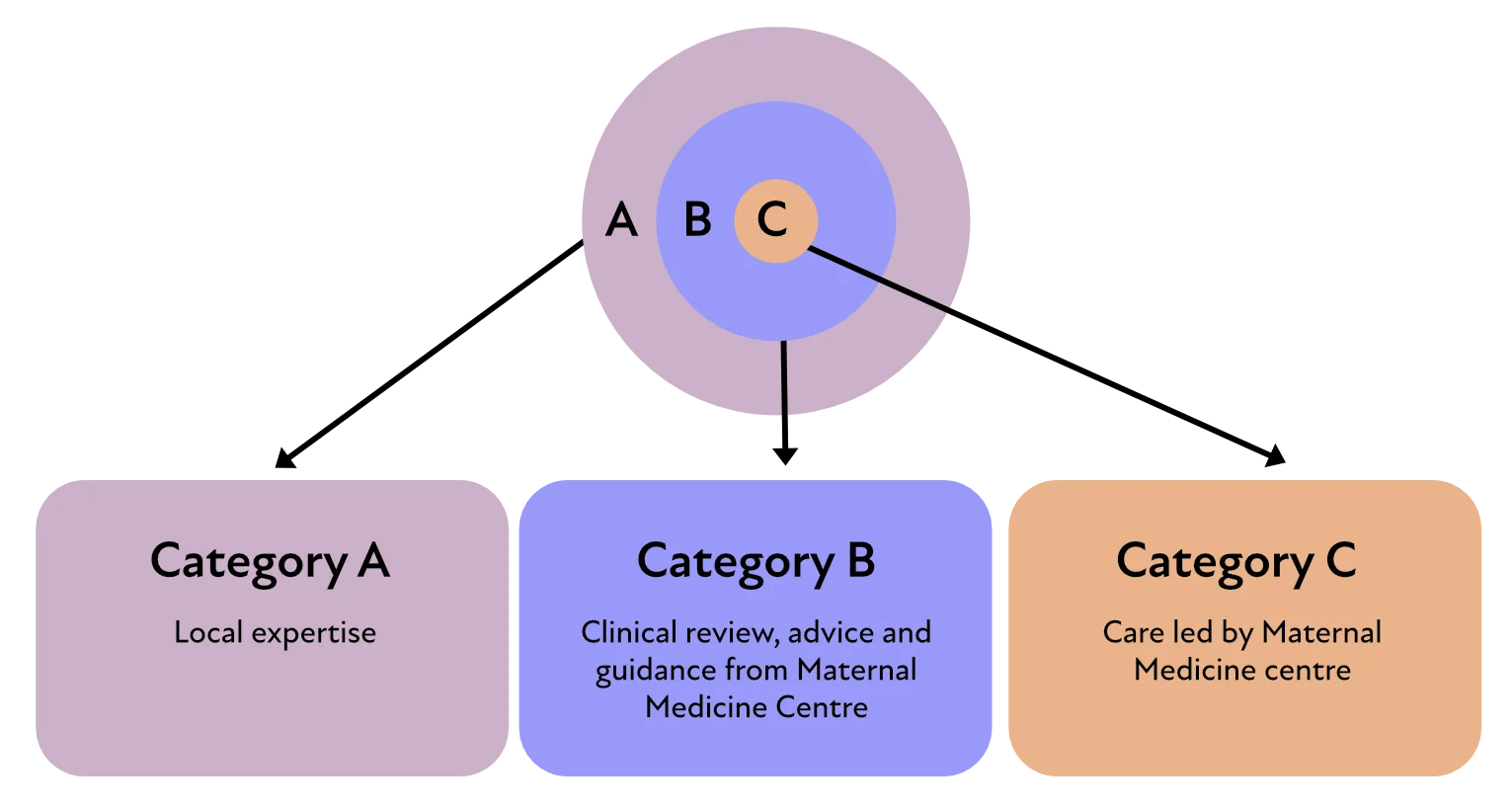
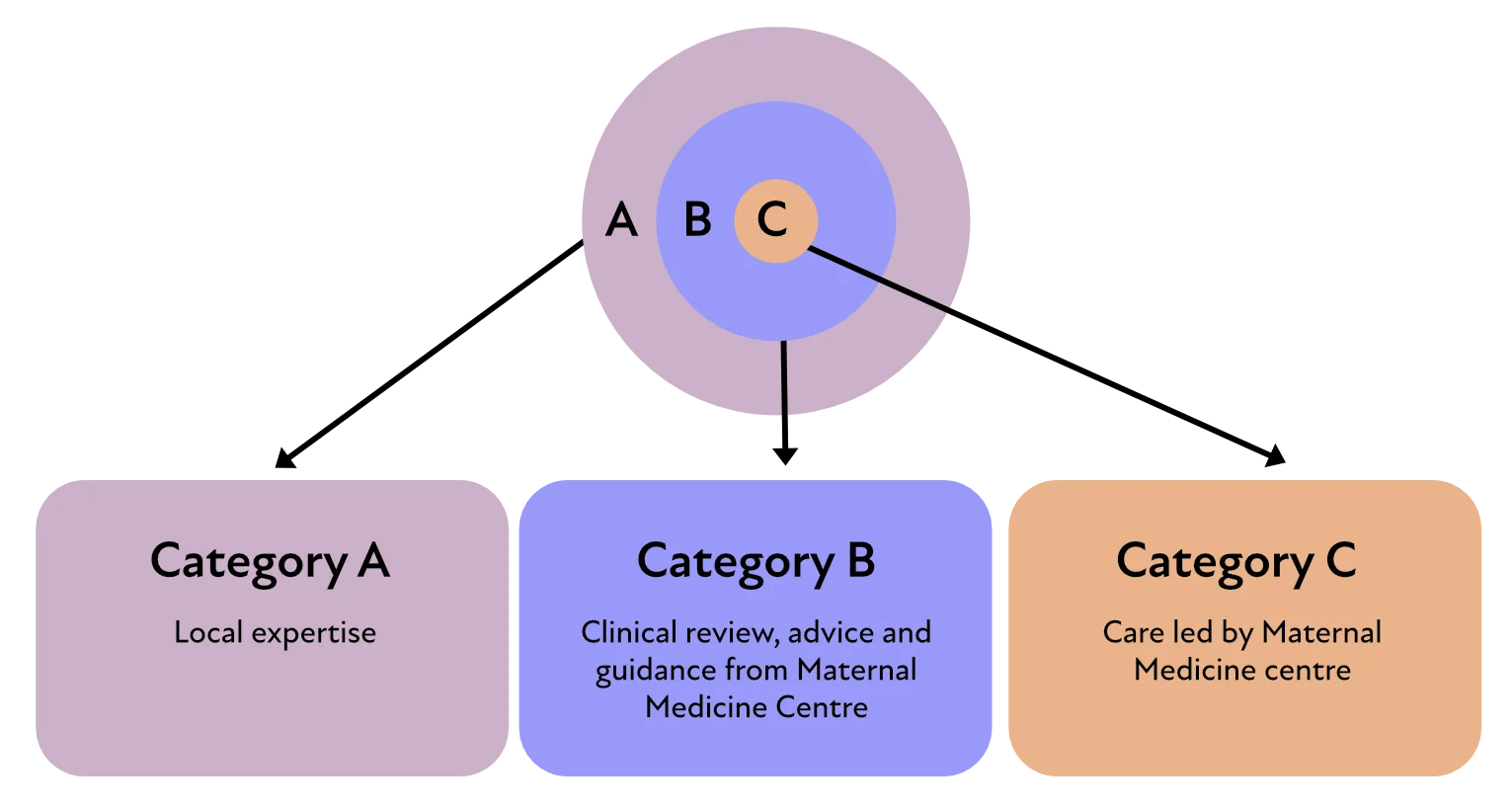
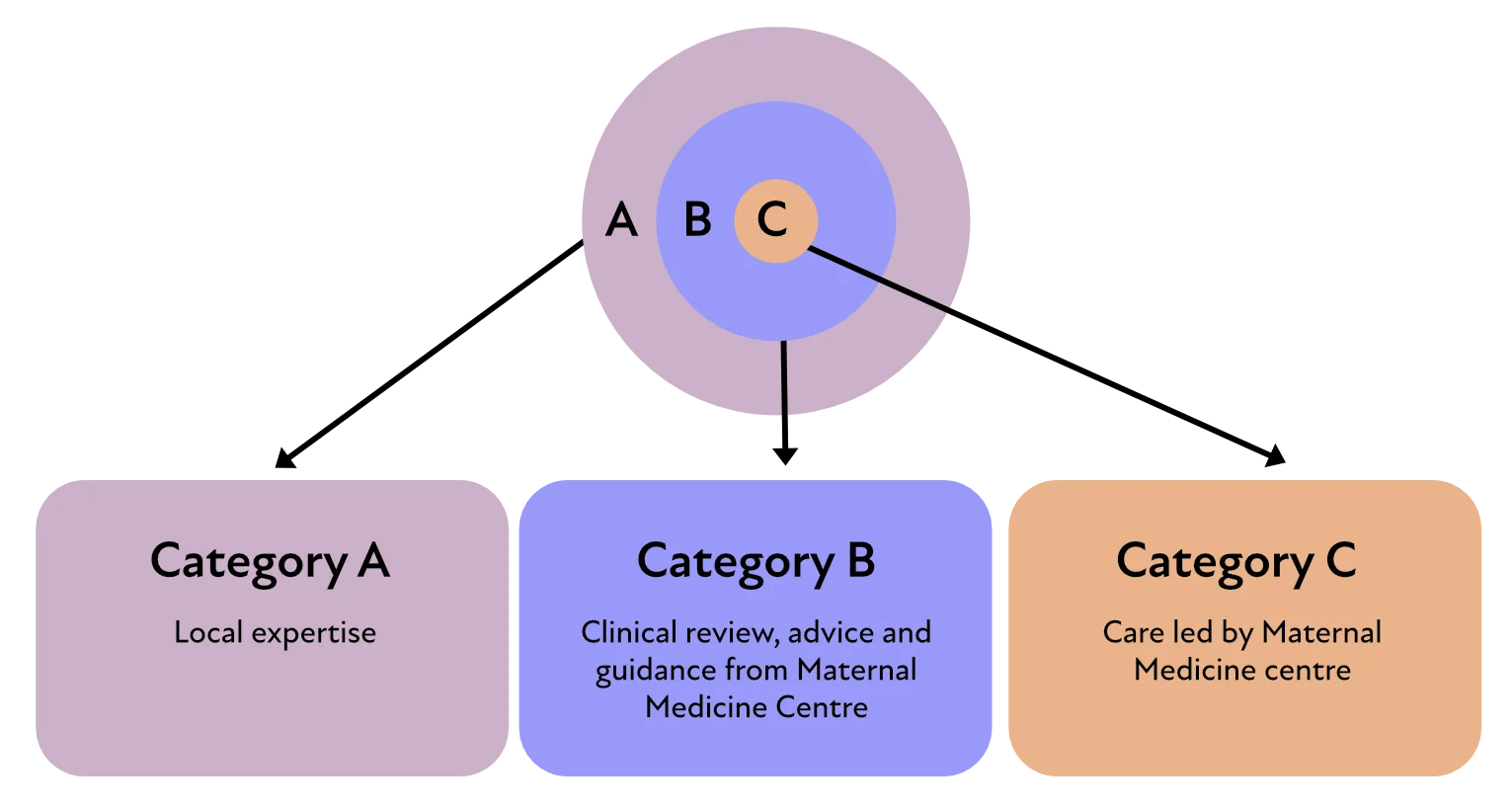
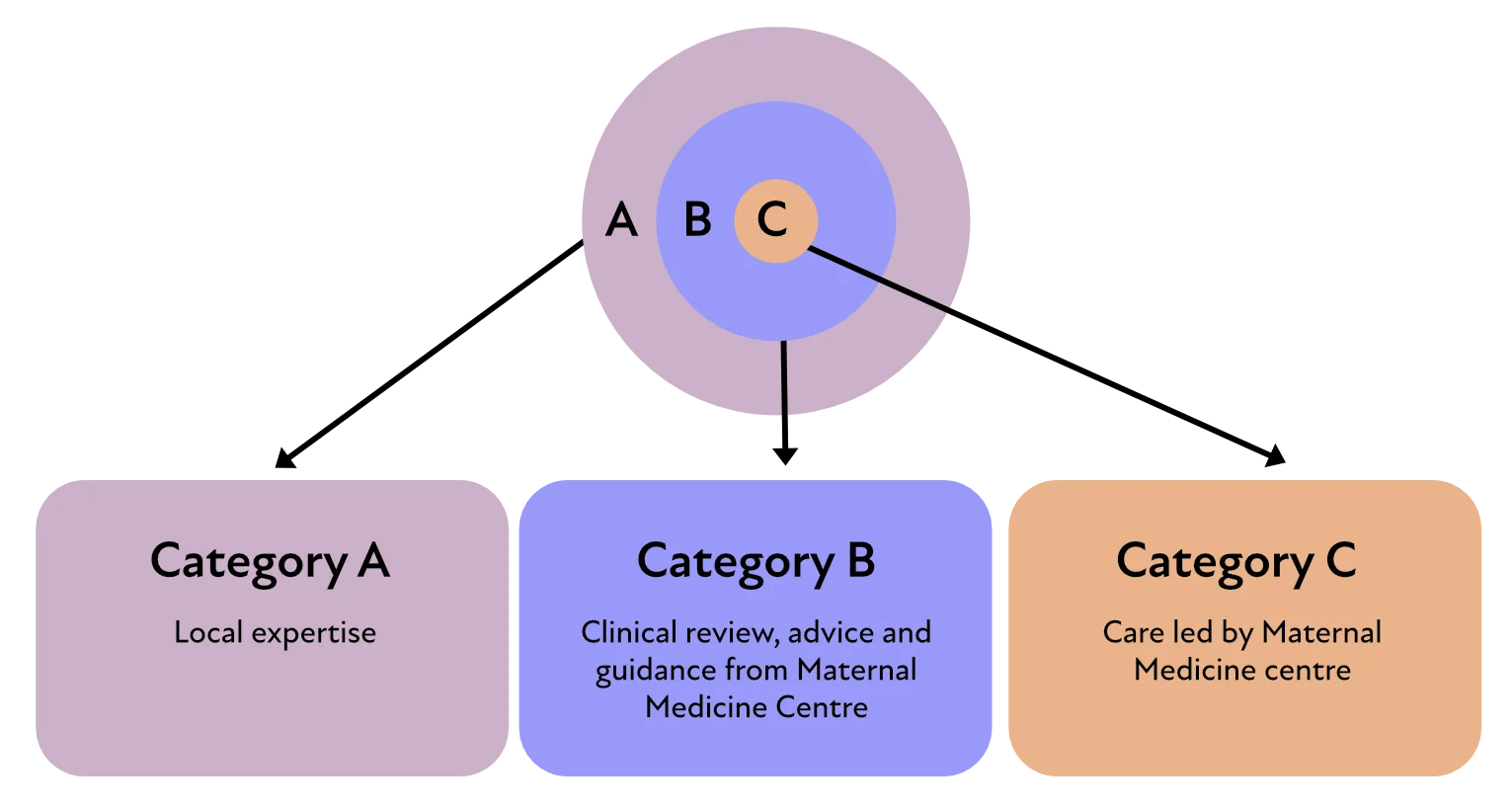
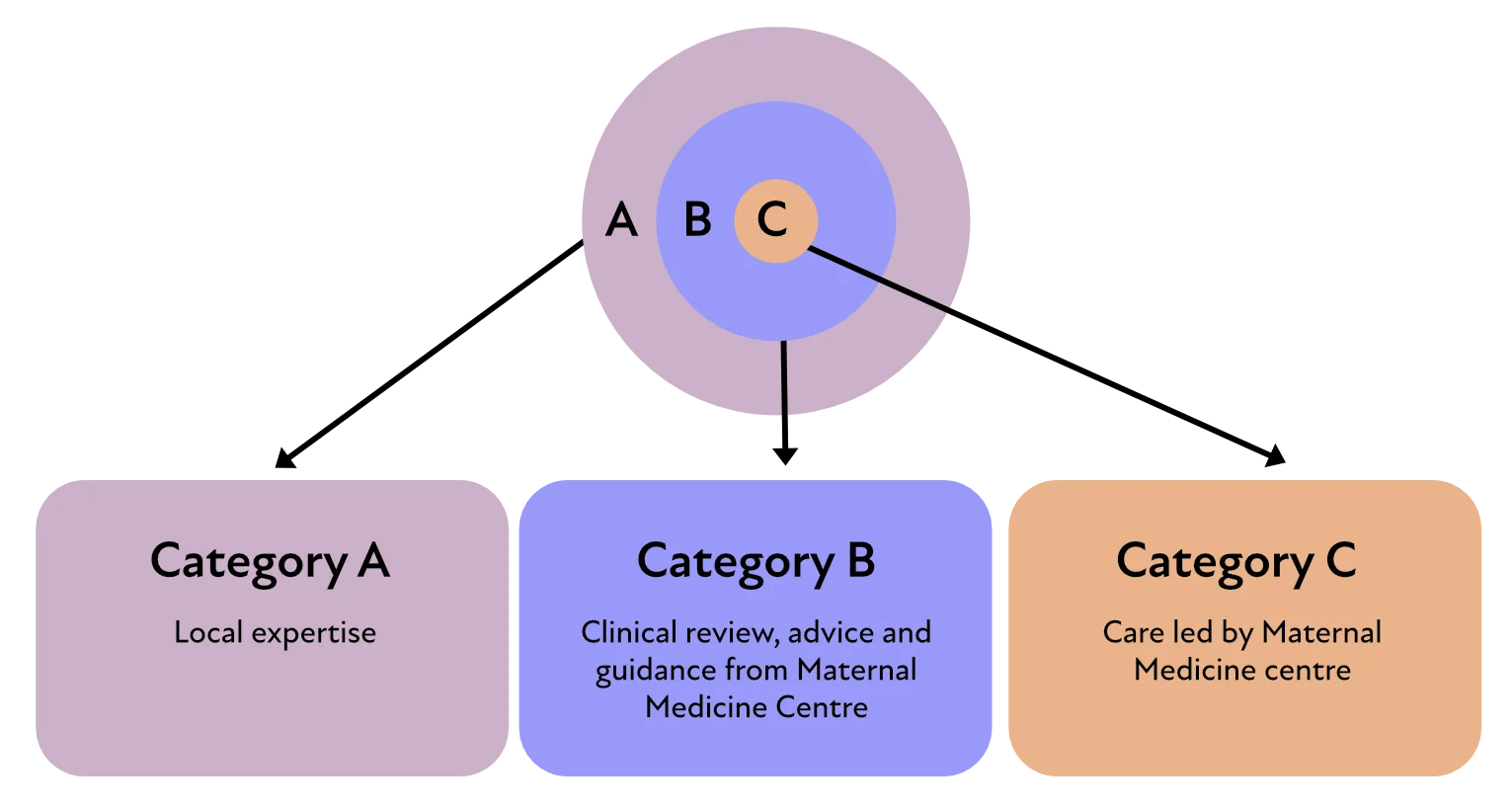
We are here to support you to look after women in a number of ways:
- Refer for advice, care or MDT opinion
- Network Guidelines and Pathways for maternal medicine conditions
- Guidance for pre-conception and post-natal care
- Evidence based clinical resources
- Prescribing support
- Resources for acute medical problems in pregnancy
- Access to continuing professional development and education
Please don’t hesitate to get in touch with any other queries.
Maternal Medicine Specialties
Please click on individual specialty boxes below for a breakdown of conditions and who to refer.
Regional MMN Speciality guidelines can be found here and pregnancy specific clinical resources for each speciality can be found here.
Cardiology
Diabetes
Rheumatology
Respiratory
Endocrinology
Neurology
Gastroenterology and Liver
Renal
Haematology
Preconceptual Care
Acute medical problems in pregnancy
Content coming soon…
Post partum care
Post-partum care covers the period immediately following birth up until approximately 6 – 8 weeks. This remains a time during which immense changes occur both in the physical and, sometimes, emotional wellbeing of the woman.
Women with medical conditions pre-existing pregnancy are particularly vulnerable post-partum, with the care and communication between the hospital specialists and their general practitioners often being fragmented. In addition, it is important that women who developed a medical condition during pregnancy, such as pre-eclampsia are followed up to ensure full resolution or monitor for any longer-term sequelae of that condition.
Medications
Prescribing or continuing medications in pregnancy is a cause for significant concern and anxiety for health professionals for fear of causing harm to the fetus. However, it is important to also consider the risks of not adequately treating the underlying condition as this can have an impact on both the woman and developing fetus. For example, we know that uncontrolled autoimmune disease is associated with a higher risk of preterm birth, fetal growth restriction, preeclampsia, venous thromboembolism, and other pregnancy complications.
Therefore, you need to balance the risks and benefits of starting/continuing the medication against the risks and benefits of stopping or withholding them.
Unfortunately, there is a lot of outdated and misguided information with regards to medication, and very few medications are licensed in pregnancy. However, many medications are safe to continue in pregnancy. It is important to refer to and use reputable evidence-based resources and guidelines to adequately inform and counsel the woman on the safety of medications in pregnancy.
Please see links for recommended resources for information on prescribing in pregnancy and breastfeeding.
Research into the effects of taking different medications is a slow growing field. Here are some resources that bring together existing knowledge:
This website provides reliable, evidence-based, and accurate information about use of medicines in pregnancy, in the form of freely available patient information leaflets called ‘Bumps‘ (‘Best Use of Medicines in Pregnancy’).
.
This is effectively the professional’s version of bumps. It is free but requires registration
Cardiology
| mWHO I | mWHO II | mWHO II-III | mWHO III | mWHO IV | |
|---|---|---|---|---|---|
| Diagnosis (if otherwise well and uncomplicated) |
Small or mild – pulmonary stenosis – patent ductus arteriosus – mitral valve prolapse Successfully repaired simple lesions (atrial or ventricular septal defect, patent ductus arteriosus, anomalous pulmonary venous drainage) Atrial or ventricular ectopic beats isolated |
Unoperated atrial septal or ventricular defect Repaired tetralogy of Fallot Most arrhythmias (supraventricular arrhythmias) |
Mild left ventricular impairment (EF >45%) Hypertrophic cardiomyopathy Native or tissue valve disease not considered WHO I or IV (mild mitral aortic stenosis) Marfan or other HTAD syndrome without aortic dilatation Aorta <45 mm in bicuspid aortic valve pathology Repaired coarctation Atrioventricular septal defect Turners Syndrome All channelopathies (event rate not applicable) |
Moderate left ventricular impairment (EF 30-45%) Previous peripartum cardiomyopathy without any residual impairment of left ventricular function Systemic right ventricle with good or mildly decreased ventricular function Fontan circulation. If otherwise the patient is well and the cardiac condition uncomplicated Unrepaired cyanotic heart disease Other complex heart disease Moderate mitral stenosis Severe asymptomatic aortic stenosis Moderate aortic dilatation Ventricular tachycardia |
Pulmonary arterial hypertension (managed in Sheffield PH service) Severe left ventricular dysfunction (EF <30% or NYHA class III-IV) Previous peripartum cardiomyopathy with any residual left ventricular impairment Severe mitral stenosis Severe symptomatic aortic stenosis Systemic right ventricle with moderate or severely decreased ventricular function Severe aortic dilatation Vascular Ehlers-Danlos Severe (re)coarctation Fontan with any complication Mechanical valve |
| Risk | No detectable increased risk of maternal mortality and no/mild increased risk in morbidity | Small increased risk of maternal mortality or moderate increase in morbidity | Intermediate increased risk of maternal mortality or moderate to severe | Significantly increased risk of maternal mortality or severe | Extremely high risk of maternal mortality or severe |
| Maternal cardiac event rate |
2.5-5% | 5.7-10.5% | 10-19% | 19-27% | 40-100% |
| Pre-pregnancy Counselling |
Optional- local unit | Yes-local unit | Yes- local unit | Yes: expert counselling required |
Yes: expert counselling required |
| Care during pregnancy | At the Local hospital. If there are concerns, or a lack of expertise or timely review in the local hospital, refer to the obstetric cardiology clinic at the local MMC forreview or advice. | At the Local hospital. If there are concerns, or a lack of expertise or timely review in the local hospital, refer to the obstetric cardiology clinic at the local MMC for review or advice. | Refer to the Obstetric Cardiology Clinic at the local MMC for MDT consideration about where antenatal care and delivery is most appropriately located irrespective of where they usually attend for their cardiac care. For some women, delivery may be appropriate in their local unit. | Refer to the Obstetric Cardiology Clinic at the local MMC for MDT consideration about where antenatal care and delivery is most appropriately located irrespective of where they usually attend for their cardiac care. |
Refer to the Obstetric Cardiology Clinic at their local MMC for regional MDT discussion and decision about transfer of antenatal care and delivery. Pulmonary Hypertension cases discussed in MMC MDT -managed in Sheffield PH Service |
| Minimal follow-up visits during pregnancy |
Once or twice | Once per trimester | Bimonthly | Monthly or Bimonthly | Monthly |
| Location of delivery | Local hospital | Local Hospital or Individualised assessment after MDT review | Individualised assessment after MDT review | Expert centre for pregnancy and cardiac disease as decided at MMC MDT review | Expert centre for pregnancy and cardiac disease as decided at MMC MDT or Regional MDT |
Respiratory
| Uncomplicated Asthma |
Complicated asthma:
|
Sickle chest crisis (see Haematology pathway) |
| Pneumonia | Restrictive lung disease (eg ILD, kyphoscoliosis) with FVC >50% |
Restrictive lung disease (eg ILD, kyphoscoliosis) with FVC <50% |
| TB | Any respiratory condition receiving immunotherapy / biologics | Neuromuscular disorders with respiratory muscle involvement eg myasthenia gravis, Guillain-Barré syndrome |
| Chronic Obstructive Airways Disease | Bronchiectasis | Cystic fibrosis |
| Pneumothorax | New diagnosis of obstructive sleep apnoea/obesity hypoventilation in pregnancy | Lung transplant |
| Sarcoidosis without restrictive lung disease, no renal involvement | COVID pneumonitis | Pulmonary vasculitis |
| Managed obstructive sleep apnoea/obesity hypoventilation | Lung cancer | |
| Pulmonary embolus (see Haematology pathway) |
Gastroenterology and Liver
| Hyperemesis gravidarum | Complex inflammatory bowel disease:
|
Portal hypertension |
| Constipation | Acute and chronic pancreatitis | Complex pancreatitis
|
| Gallstones | Treated GI malignancy | Active malignancy |
| Gastro-oesophageal reflux disease | Unexplained jaundice | Cirrhosis |
| Coeliac disease | Acute fatty liver of pregnancy | Decompensated liver disease/liver failure* |
| Viral hepatitis | Achalasia | Liver transplant |
| Intrahepatic cholestasis (bile acids <100) | Intrahepatic cholestasis (bile acids ≥100) | |
| Uncomplicated inflammatory bowel disease in remission | Liver infarction/haematoma | |
| Cholecystitis | Autoimmune hepatitis | |
| Viral hepatitis | Wilson’s disease | |
| HELLP | Crigler Najjar syndrome | |
| Primary biliary cirrhosis | ||
| Primary sclerosing cholangitis |
Diabetes
|
Gestational diabetes mellitus |
Diabetic nephropathy – Nephropathy Creatinine >70mmol/l or PCR >30 mg/mmol |
Diabetic nephropathy – creatinine >120 or PCR >300 mg/mmol |
|
Type I and II diabetes mellitus without complications or co-morbidities |
Diabetic retinopathy requiring treatment during pregnancy (where local ophthalmology services are not providing treatment) |
Complex diabetic retinopathy requiring treatment (significant nephropathy likely to coincide) |
|
Autonomic neuropathy causing significant complications eg. gastroparesis |
Cardiovascular complications e.g. Congenital or acquired cardiac diseases, Cerebrovascular diseases, Resistant hypertension |
|
|
Monogenic diabetes |
Endocrinology
| Hypothyroidism | Thyroid hormone resistance | Primary and secondary hyperaldosteronism |
| Hyperthyroidism and gestational hyperthyroidism | Thyroid cancer | Phaeochromocytoma or paraganglioma |
| Thyroid nodules | Macroprolactinoma | Cushing’s syndrome |
| Microprolactinoma | Pituitary disease on hormone replacement therapy | Acromegaly |
| PCOS | Congenital adrenal hyperplasia | Metabolic disorders such as Glycogen storage disorder |
| Vitamin D deficiency | Dumping syndrome post bariatric surgery | Hyperparathyroidsm |
| Addison’s disease | Hypoparathyroidism |
Renal
| Single kidney | Lupus nephritis in remission or on treatment | Active lupus nephritis |
|
Non-lupus glomerulonephritis/ tubulointerstitial nephritis:
|
Non-lupus glomerulonephritis/ tubulointerstitial nephritis:
|
Pre-pregnancy CKD stages 4 and 5 |
| Kidney stones | Kidney transplant | Combined kidney-pancreas transplant |
| Recurrent UTI no immunosuppression | Recurrent UTI on immunosuppression | Dialysis |
| Reflux nephropathy with normal kidney function | Reflux nephropathy with abnormal kidney function | New renal vasculitis in pregnancy and vasculitis on immunosuppression |
| Autosomal dominant polycystic kidney disease with normal kidney function. | Autosomal dominant polycystic kidney disease with abnormal kidney function | Scleroderma renal crisis |
| AKI responding to treatment | AKI not responding to treatment or not resolving post-partum | |
| AKI due to pre-eclampsia resolved post-partum | Previous renal vasculitis in remission, no longer on treatment | |
| Previous urinary tract reconstructive surgery | ||
| Kidney disease requiring OR on biologic treatment | ||
| Progressive kidney disease in pregnancy |
Rheumatology
| Uncomplicated rheumatoid arthritis | Rheumatological disease requiring biologic therapy | Active lupus nephritis (see Kidney Pathway) |
Uncomplicated seronegative arthritis:
|
Rheumatological not controlled on current treatment | Large and medium vessel vasculitis |
Uncomplicated connective tissue disease:
|
Rheumatological disease with restrictive lung disease and FVC >50% (see Lung Pathway) | Rheumatological disease with restrictive lung disease and FVC ≤50% |
| Osteoarthritis | Rheumatological disease with kidney involvement (see Kidney Pathway) | New small vessel vasculitis or small vessel vasculitis on immunosuppression |
| Obstetric antiphospholipid syndrome (see Haematology Pathway) |
Thrombotic antiphospholipid syndrome (see Haematology Pathway) | Vascular Ehlers Danlos |
| Hypermobile Ehlers Danlos (type III) | Other Ehlers Danlos syndromes | Scleroderma renal crisis |
| Diffuse scleroderma | Antisynthetase syndrome | |
| Small vessel vasculitis in remission, no longer on treatment | ||
| Polymyositis-dermatomyositis | ||
| Behcet’s syndrome |
Neurology
| Epilepsy managed in a combined clinic including specialist neurology and obstetrics | Cluster headache | All epilepsy without local access to a combined clinic including specialist neurology and obstetrics. |
| Migraine | Idiopathic intracranial hypertension | Symptomatic raised intracranial pressure |
| Stable, small cerebrovascular malformation, reviewed within 2 years of conception, plan for mode of delivery | CVM, not reviewed within 2 years of conception |
Unstable CVM/AVM/cavernoma |
| Previous brain tumour | Current brain tumour | Progressive brain tumour |
| Previous cerebral vein thrombosis (CVT) | New cerebral vein thrombosis (CVT) | Acute stroke* |
| Meningitis | Previous Guillain Barre Syndrome | New-onset Guillain-Barre syndrome |
| Previous encephalitis | Treated, stable myasthenia gravis | New diagnosis or flare of myasthenia gravis |
| Stable multiple sclerosis managed without disease modifying drugs | Unstable multiple sclerosis or disease modifying drugs | Myotonic dystrophy |
|
Mononeuropathy eg: Bell’s palsy |
Progressive or persistent mononeuropathy | |
| Post-dural puncture headache | New encephalitis | |
| Reversible Cerebral Vasoconstriction Syndrome (RCVS) | ||
| Posterior Reversible Encephalopathy Syndrome (PRES) | ||
| Spinal cord injury | ||
| Neurofibromatosis | ||
| Neuromuscular dystrophy | ||
| Spinal muscular atrophy | ||
| Motor neurone disease |
Haematology
| Sickle cell trait | Current immune thrombocytopenia and platelet count ≤75 | Sickle cell disease |
| Historical immune thrombocytopenia and platelet count >75 | Thrombocytosis | Beta thalassaemia major |
| Gestational thrombocytopenia | White cell disorders |
Other complex thalassaemia:
|
| Current VTE or previous single VTE | Recurrent VTE | Current extensive VTE without other access to Factor Xa monitoring |
| Obstetric antiphospholipid syndrome | Thrombotic antiphospholipid syndrome | Antiphospholipid syndrome with extensive arterial events |
| Inherited thrombophilia (no VTE, not antithrombin deficiency) | Inherited thrombophilia with previous VTE | Antithrombin deficiency |
| History of treated haematological malignancy | Stable myeloproliferative/ myelodysplastic disease | Active haematological malignancy |
| Alpha/beta thalassaemia trait |
Mild, isolated clotting factor deficiency
|
Clotting factor deficiency:
|
| B12/folate deficiency | Mild platelet function disorder with platelet count >100 | Moderate/severe platelet function disorder or with platelet count >100 |
| Carriers of haemophilia with known female fetus and normal factor VIII/IX | Carriers of haemophilia with male or unknown gender of fetus | |
| Type I Von-Willebrand disease, VWF activity normalised in pregnancy | Von-Willebrand disease:Type 1 if VWF not normalised,Type II &Type III | |
| Transfusion dependent disease |