Maternal Medicine Networks
Maternal Medicine Networks (MMN)
are central to NHS England’s Improvement plan for supporting all pregnant women and their babies. The aim of MMNs is to ensure women with medical conditions have timely access to the best specialist advice and care at all stages of their pregnancy.
Medical disease relevant to a maternal medicine service includes but is not limited to:
- Cardiac disease
- Respiratory disease • Renal disease
- Haematology
- Rheumatological disease
- Endocrine disease
- Gastrointestinal and liver disease
- Neurological disease • Skin disease
- Cancer
It also includes acute illness where the underlying condition is not clear, such as:
- Headache
- Breathlessness
- Chest pain
- Abdominal pain
- Fever/sepsis


MMNs provide clinical leadership for the identification, referral and management of women and their medical conditions within the network, with identified Maternal Medicine Centres (MMC) having responsibility for co-ordinating the care required for women who use the services. MMNs encourage specialist doctors, midwives and nurses to work together to improve pre -pregnancy counselling and optimise medical care.
Aim of the service:
- To provide advice and planned care for women with pre -existing medical conditions, before, during and after pregnancy – ensuring equitable access, excellent experience and optimal outcomes for all communities served by the service.
- To provide advice and planned intrapartum and postpartum care for women with medical conditions that arise during pregnancy
- To provide local clinical leadership on the identification, referral and management of women with medical conditions, including reviewing training, clinical guidelines and referral pathways for all staff in contact with pregnant women across the footprint.
- To reduce inequities in pregnancy outcomes relating to medical complexity across all demographics
Identifying women at risk
Recent MBRRACE reports from the confidential enquiries into maternal deaths highlight that more woman are dying from ‘indirect’ causes (such as heart disease, neurological conditions and sepsis) than from ‘direct’ causes directly attributable to complications of pregnancy and childbirth.
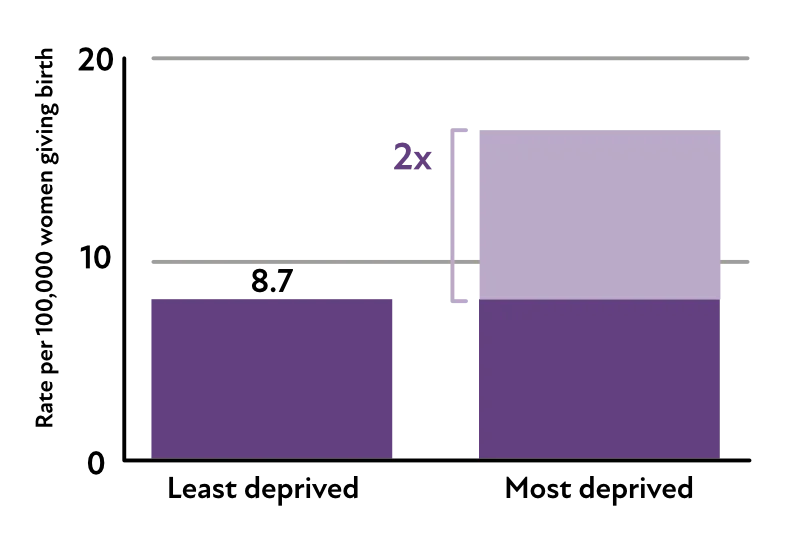
Women living in the most deprived areas continue to have the highest maternal mortality rate compared to those living in the least deprived areas:
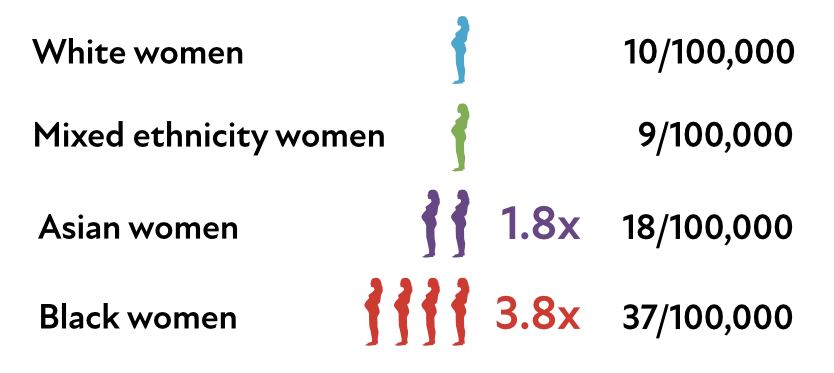
Women from Black ethnic backgrounds remain four times more likely to die, and women from Asian ethnic backgrounds are twice as likely to die, compared to White women:
Black and Asian women are at increased risk of a poor pregnancy outcome as are women who come from a more deprived social background or those with pre-existing mental health conditions.
The NW MMN is therefore pro-actively reaching out to our communities to encourage timely engagement with healthcare services and working with healthcare providers to improve access to care and increase awareness: See Co-production and Collaboration